- What is TMD?
- Do I have TMD?
- Who is at risk for TMD?
- How do you treat TMD?
- How long does it take to cure TMD?
- Does TMD / TMJ show up on an X-ray?
- Does TMD / TMJ make your chin look longer?
- What could be the issue ENT (ear, nose, and throat) or dental or TMD / TMJ?
- How to tell the difference between TMJ and arthritis?
- What should I look for in a TMD / TMJ specialist?
- What is a TMD / TMJ Specialist called?
What is TMD?
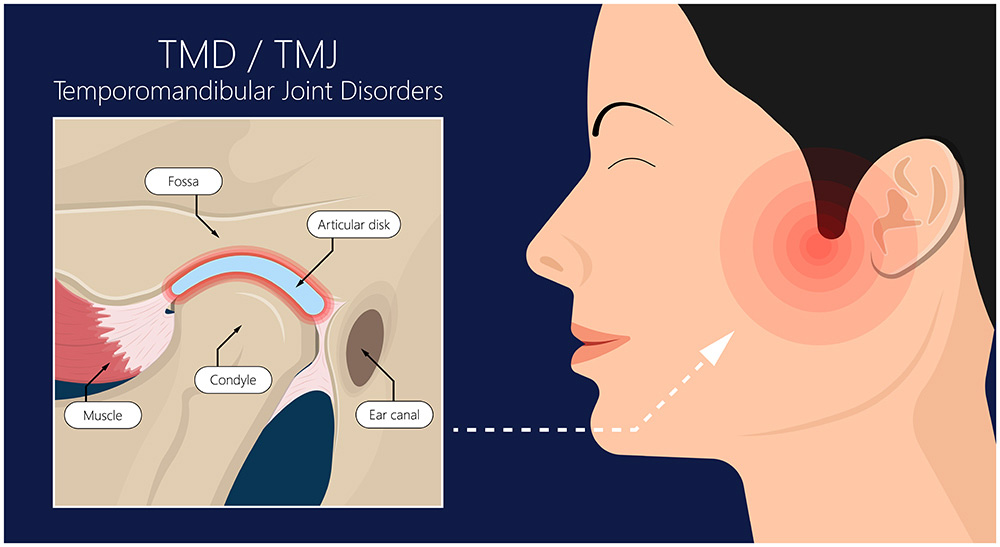
TMJ disorders encompass conditions that impact the temporomandibular joint and the associated muscles responsible for jaw movement. TMD is commonly used to describe the presence of pain, tenderness, clicking, or locking of the TMJ and the surrounding tissue.
Some symptoms of TMD include:
The causes of TMD include arthritis, joint or disk injury, teeth grinding or clenching, stress, and misalignment of teeth or the TMJ. Treatment options vary depending on the causes and may involve physical therapy, splint therapy, medications, orthodontics, surgery, stress reduction, and other approaches. It is crucial to address contributing factors for long-term relief.
Do I have TMD?
To ascertain whether you are experiencing TMD (temporomandibular joint dysfunction), it is necessary to undergo an evaluation conducted by a dental practitioner. Nevertheless, the following symptoms may serve as indicators of TMD:
The causes of TMD include arthritis, joint or disk injury, teeth grinding or clenching, stress, and misalignment of teeth or the TMJ. Treatment options vary depending on the causes and may involve physical therapy, splint therapy, medications, orthodontics, surgery, stress reduction, and other approaches. It is crucial to address contributing factors for long-term relief.
Do the symptoms of TMD / TMJ go away?
For some people with temporomandibular joint disorder (TMD/TMJ), the symptoms may entirely go away at some point. But for many, TMD symptoms instead tend to fluctuate in severity.
TMD pain and dysfunction can be managed well with suitable treatment that is customized to the specific causes. However, patients may experience symptoms such as jaw pain, difficulty chewing, locking jaw, and headaches that can recur periodically or evolve over time.
Factors influencing the progression and longevity of TMD symptoms include:
Maintaining symptom control often requires lifelong vigilance in avoiding habits that worsen the condition, consistently using nightguards and undergoing physical therapy, as well as managing any underlying conditions that contribute to TMD.
Who is at risk for TMD?
Certain risk factors increase an individual’s susceptibility to developing temporomandibular joint dysfunction (TMD). Below, you will find some of the primary factors associated with this condition:
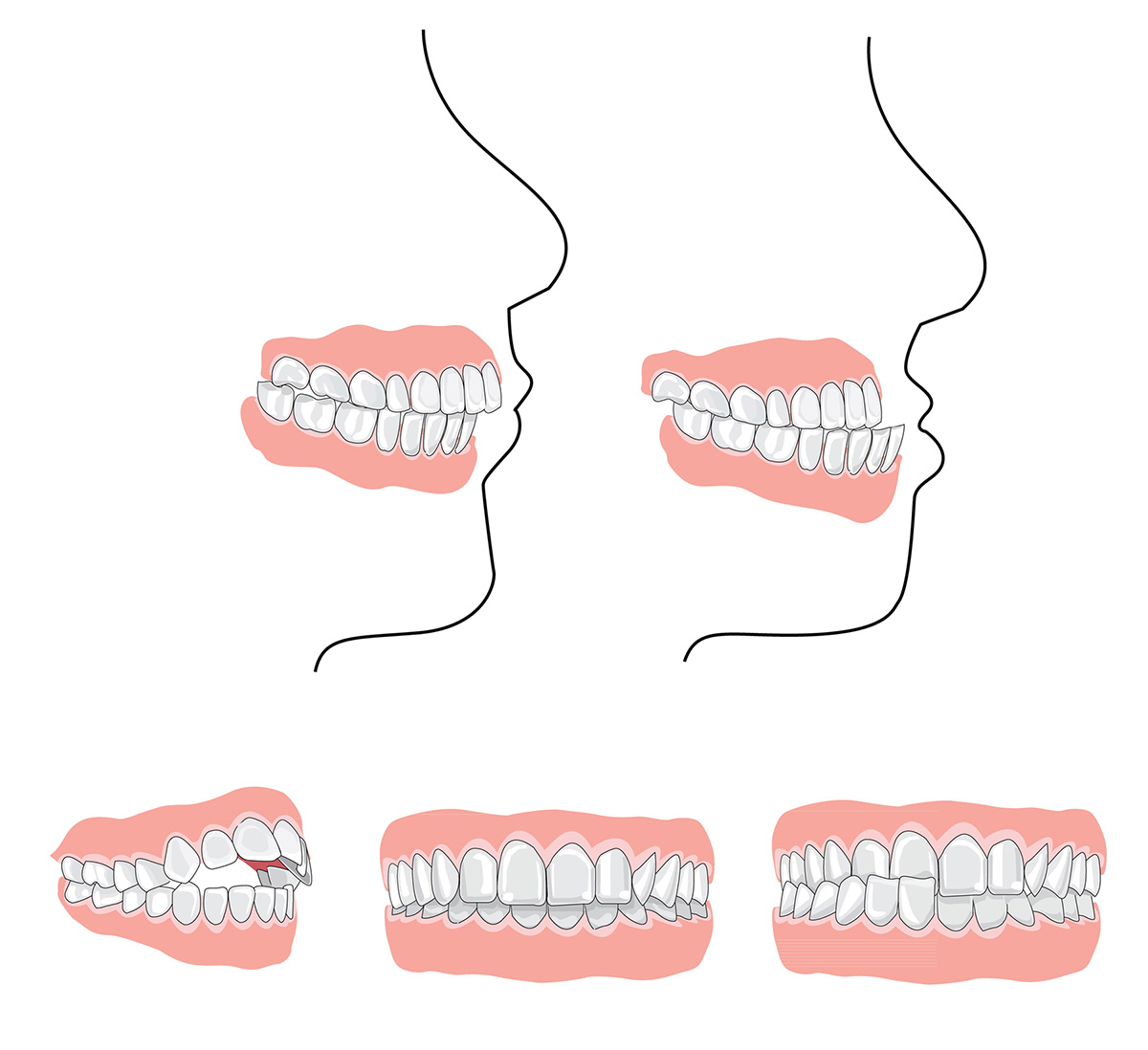
Misaligned Bite
If you have any of those TMD risk factors, get evaluated promptly when noticing pain on chewing or other odd jaw symptoms arise. The earlier treatment begins, the more manageable symptoms become.
How do you treat TMD?
The following are some therapies you can do to treat TMD:
1. Keep your jaw in a resting position
Overuse of the jaw can cause issues for those who suffer from TMD. Maintaining a resting position with your jaw gives the joint a chance to relax and fall back into place.
Minimizing certain activities like:
These activities can cause added pain to your TMJ.
To relieve some of the pain, keep your teeth apart slightly and keep the clenching and grinding to a minimum.
2. Apply a cold or hot compress
Using a hot or cold compress works for all muscle pain, including the joints and muscles in the jaw. It is recommended to use heat in the area in the mornings to increase blood flow and relax the jaw to prepare it for the day.
Likewise, using an ice pack at night is beneficial to help bring down any swelling or pain accumulated throughout the day. It is recommended to apply these compresses for 15 to 20 minutes, no longer. Make sure you use a cloth to add a layer of protection between the compress and your skin.
3. Take steps to reduce stress
TMD is most common for those who excessively grind and clench their teeth. In some cases, this can be caused by increased stress and anxiety. This anxiety can cause pressure and pain in the jaw joints due to consistent cleaning.
It is best to try meditation, yoga, and other forms of stress reduction like gardening or reading to calm yourself from day-to-day anxieties.
Massages are also a great way to reduce stress and tension in the body, including the jaw muscles.
4. Avoid certain foods and increase others
Hard and sticky foods can directly impact the pain you feel in your jaw due to TMJ. When you need to exert a lot of force to chew a piece of food, you will put your jaw in the wrong position.
As stated before, chewing is top of that list with activities to stay away from, like yawning and yelling.
Avoid foods that are hard and crunchy, including large pieces of ice.
Chewing gum can also pose an issue since there is constant mastication occurring.
Start eating soft foods like mashed potatoes, yogurt, pudding, beans, etc., so chewing is minimal.
5. Utilize over-the-counter medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) help alleviate pain and swelling in an individual’s muscles.
These medications are usually over-the-counter, like naproxen or ibuprofen, but depending on pain, your dentist may be able to prescribe you a higher dose.
Alongside muscle relaxants, you could also be prescribed medications to help relieve stress to help with the clenching and grinding to ease anxiety. But, again, speak with your doctor about your options depending on your pain level.
How long does it take to cure TMD?
There is no defined cure or timeline for resolving symptoms of TMD (temporomandibular joint disorder), as durations depend greatly on the underlying cause and severity. However, with proper treatment most patients find effective relief within 6-12 months.
In the short term, non-invasive treatments focused on pain relief, joint mobilization, anti-inflammatory medications, physical therapy, or bite splints can ease discomfort significantly within the first 1-3 months already.
Longer-lasting TMD reduction relies on addressing contributory issues like teeth grinding and arthritis through night guards, occlusal adjustment, surgery, injections, stress relief practices, etc. Improvement accelerates by minimizing strain to the TMJ area once destabilizing factors are corrected.
While some minor symptoms can linger long-term or resurface if destructive habits resume, dedicated TMD therapy brings most patients significant restoration of normal jaw/chewing function within a year. Sustained improvement is observable as muscle function stabilizes, inflammation resolves and the bite stabilizes.
With tailored treatment plans closely monitored and adjusted as needed, patients find their healing trajectories highly personalized. However substantial gains are achievable once destabilizing forces are corrected.
Does TMD / TMJ show up on an X-ray?

Yes, signs of temporomandibular joint disorder (TMD/TMJ) can potentially show up on certain x-ray images, though it depends on the type and severity of damage. Here are some key points:
So in summary, while dental X-rays have minimal diagnostic value for spotting early-stage TMD, advanced CT and MRI allow clearer visibility of anatomical abnormalities, asymmetry, and tissue damage helping guide appropriate treatment courses.
Does TMD / TMJ make your chin look longer?
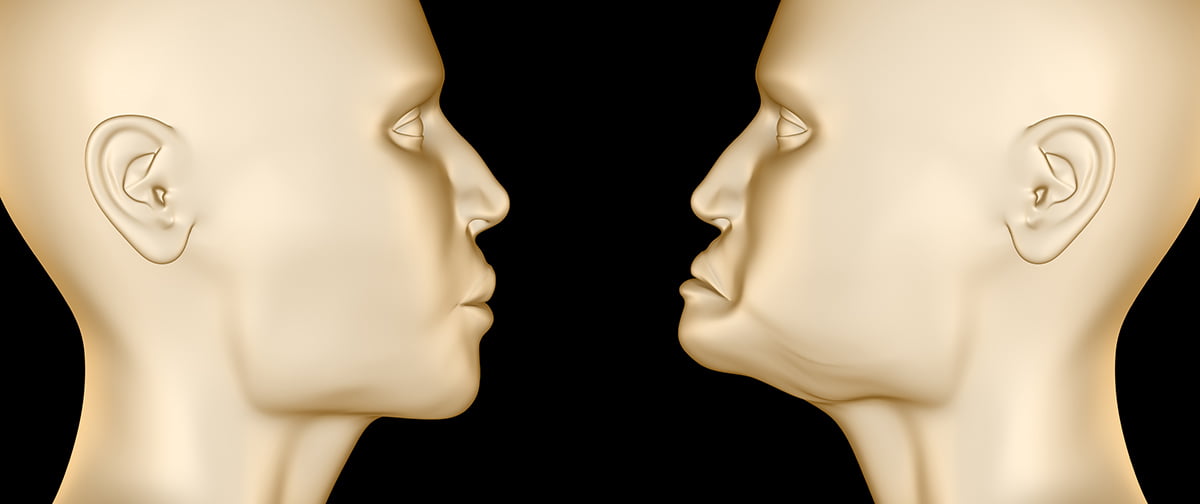
Yes, moderate to severe cases of temporomandibular joint disorder (TMD/TMJ) can sometimes make your chin look longer or more pronounced.
Here’s why:
As the jaw joint degenerates and becomes dysfunctional, the alignment between the upper and lower teeth frequently worsens. When back molars no longer meet properly, front teeth over-close to make up for gaps in the back.
This excessive vertical extension of the lower jaw necessary to have the opposing back teeth barely meet gives the appearance of a more exaggerated, protruded chin. It’s the lower jaw extending downward and forward more than usual to find a point of precarious occlusion amidst joint deterioration.
In effect, bite collapse from unchecked TMD literally lengthens facial height. As misalignment progresses uncorrected, the lips have increased difficulty meeting as well which further stretches chin tissue downward.
Re-establishing harmonious occlusion through techniques like bite splints or selective teeth removal relieves strain which may reverse chin elongation to some degree over time as bite stability returns.
What could be the issue ENT (ear, nose, and throat) or dental or TMD / TMJ?

Differentiating between ENT, dental, and TMD/TMJ sources can be challenging when patients experience overlapping face, jaw or headache symptoms.
Here are tips to uncover the likely primary issue:
While connections exist between ears, dental occlusion, and jaw joints, targeted symptoms provide clues to primary offenders. But comprehensive evaluations with a team of specialists teasing apart contributions are essential, as advanced multidisciplinary care achieves the best patient outcomes long term.
How to tell the difference between TMJ and arthritis?
There are some distinct differences in symptoms and exam findings that help differentiate between TMJ (temporomandibular joint) disorders versus types of inflammatory arthritis affecting the jaw joint areas:
TMD / TMJ Dysfunction Signs
Arthritis symptoms
While some findings occasionally overlap, the location of discomfort, the exacerbating and relieving factors, the presence of fever/swelling/inflammation, and timing pain patterns all help guide appropriate diagnosis – either TMJ issues or inflammatory arthritis.
Specialized testing like joint fluid analysis and imaging also facilitates correct treatment.
What should I look for in a TMD / TMJ specialist?

When seeking a specialist for treating temporomandibular joint disorder (TMD/TMJ), look for these key qualifications and traits:
1. Training and experience
2. Holistic and individualized treatment planning
3. Strong communication skills
4. Care coordination
5. Patient focus
A skilled TMD specialist conducts a thorough examination of underlying factors and customizes treatment plans based on individual requirements, acting as a consultant rather than merely a technician.
What is a TMD / TMJ Specialist called?
A TMD / TMJ specialist is often called an orofacial pain specialist or temporomandibular disorder (TMD) specialist. Some other names they may go by include:
These all denote professionals who have advanced skills and focus specifically on evaluating and treating temporomandibular joint issues, jaw dysfunction, and face/head pain related to the mouth, jaws and skull structures.
In addition to complex TMD expertise, they incorporate wider anatomical perspectives of the cervical spine, nervous system pathways, and psychology around chronic pain. Addressing the multifactorial components of TMJ disorders requires expanded qualification.
Temporomandibular Joint Disorder is serious and painful. Speak with your dentist about your options, and be sure to implement the above into your daily routine.
 Written by Dr. Reza Khazaie
Written by Dr. Reza Khazaie